MANDATORY CONTRACTS AND TEXAS MEDICAID – OLD
Texas Medicaid is being threatened by local governments and their health plans — which receive Mandatory Contracts that force the most vulnerable Texans to seek care from some of the state’s lowest-ranked plans.
Only the Texas Legislature can fix this situation.
An out-of-date state law automatically grants Medicaid contracts to health plans controlled by county commissioners courts. These county-controlled plans are owned by — and create revenue for — local governments that tax constituents to support public hospitals.
An outdated state law says that only county-controlled plans get Mandatory Contracts worth tens or hundreds of millions of dollars — no matter how poorly they perform.
The Texas Health & Human Services Commission (HHSC) has warned that the law could force the most vulnerable Texans to seek care from “unqualified and incompetent” health plans.
SB 651 (by Sen. Charles Perry) and HB 2401 (by Rep. Tom Oliverson) would repeal this anticompetitive law, protect the most vulnerable Texans, and level the playing field in Texas Medicaid.
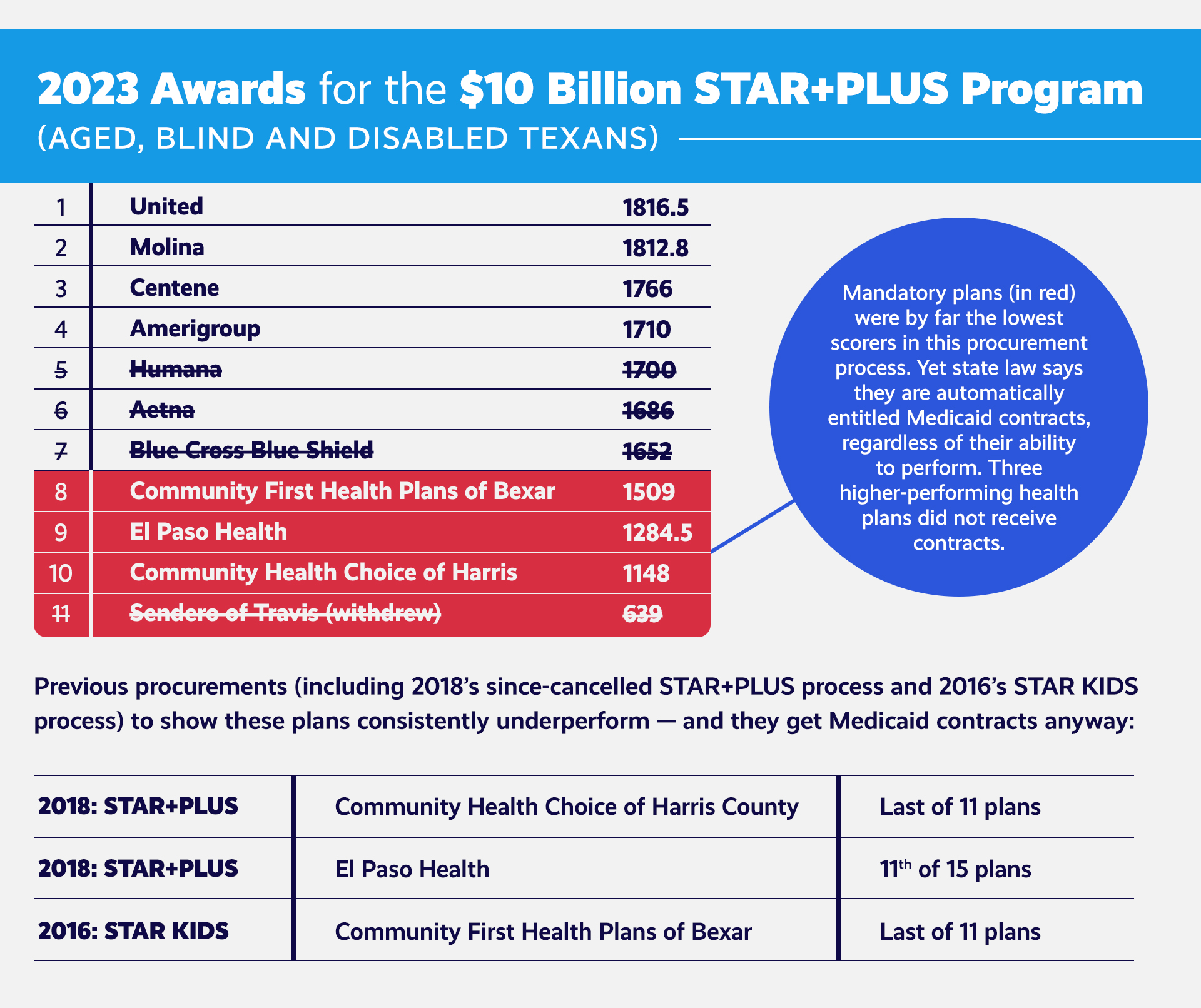
The Texas Health & Human Services Commission (HHSC) recently announced Medicaid contract awards for the state’s STAR+PLUS Program, which cares for aged, blind, and disabled Texans.
- Once again, the lowest-scoring health plans — which HHSC says are least capable of operating the program effectively — received contracts to serve Texans in key urban areas.
- Those plans are controlled by urban county commissioners courts, the governing bodies for Texas counties.
- HHSC also has stated it plans to award Mandatory Contracts in the STAR Kids and STAR and CHIP programs — which are specifically designed to serve vulnerable Texas children — to local government plans, regardless of those plans’ scores in the procurement process.
Texas courts have ruled that a law passed 24 years ago — through a floor amendment with no debate — requires HHSC to award Medicaid contracts to health plans controlled by urban county governments.
- Three years ago, HHSC tried to deny a contract to a low-performing plan overseen by the Harris County Commissioners Court.
- In response, the Harris County-controlled health plan sued the state.
- Courts ruled that Texas’ Mandatory Contracts law requires HHSC to award contracts to these plans.
In 2019, one county-controlled health plan received the lowest score, among all applicants, in the state’s procurement process for the STAR+PLUS program. HHSC rightly decided not to award the contract to that plan.
- The county-controlled health plan in turn sued the state, arguing that HHSC could not deny them business, no matter what procurement scores they received.
- The case went to the Texas Supreme Court. In its brief, the State of Texas argued that this reading of the law “deprives the Commissioner not only of the discretion, but the duty entrusted to her by the Legislature, necessary to protect the health and welfare of disabled and senior Texas citizens from unqualified and incompetent MCOs.”
- Nevertheless, Texas courts upheld Mandatory Contracts law.
County-controlled health plans have defended their exclusive standing:
- Some districts say they don’t have needed staffing to respond to HHSC Requests for Proposals.
- This begs the question about other basic functions they cannot perform.
- Some urban counties have invoked their indigent (or uninsured) care policies, claiming that local hospital districts will see less money if Mandatory Contracts are repealed.
- This argument shows that Mandatory Contracts are, first and foremost, an anticompetitive, revenue-generating mechanism for hospital districts already taxing their citizens.
- It ignores the fact that anti-competitive preferences for substandard, inadequate health plans have nothing to do with the provision of indigent care.
- Some districts have threatened to stop providing local matching funds to draw down Medicaid money through the Intergovernmental Transfers (IGT) process if their low-performing plans don’t receive Mandatory Medicaid Contracts.
- This is an empty threat, given the need for this money in these communities.
- It also carries dangerous repercussions, given the critical coordination required to secure these needed resources.
- Regardless, the drawdown of federal Medicaid dollars and the state’s IGT process have nothing to do with Mandatory Contracts for government-controlled health plans.
This year, the Texas Legislature has the opportunity to repeal the anti-competitive, out-of-date state law guaranteeing Medicaid business to underperforming health plans.
Upholding Mandatory Contracts means disregarding the poor performance of health plans controlled by hospital districts and urban county commissioners and delivering substandard care to some of Texas’ most vulnerable communities.
Just this year, Texas awarded mandatory contracts to three hospital district plans that all scored the lowest in HHSC’s procurement process:
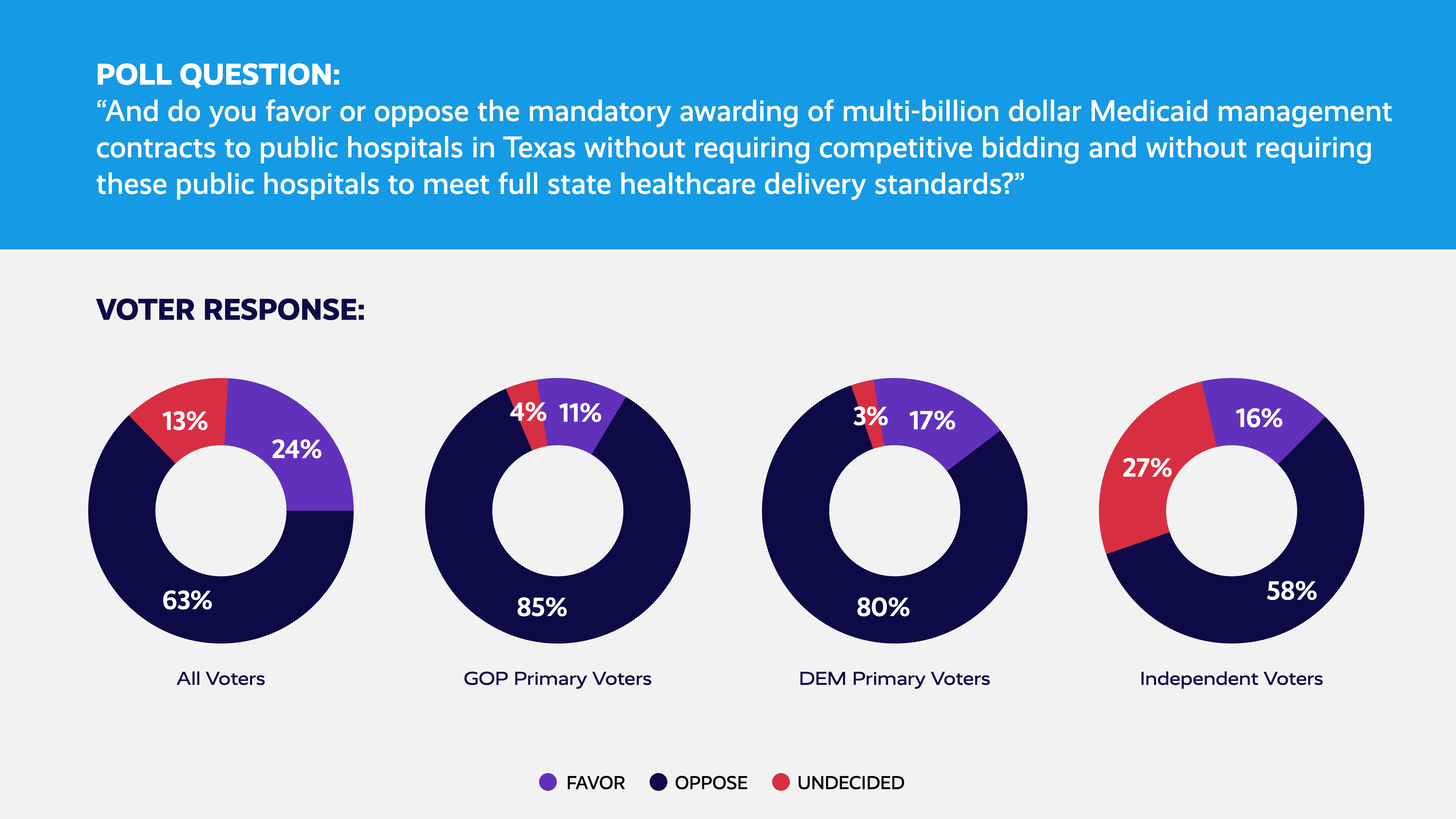
Regardless of their political party, Texans overwhelmingly oppose awarding Medicaid contracts without competitive bidding or requirements that bidders — including public hospital districts — meet full state standards.
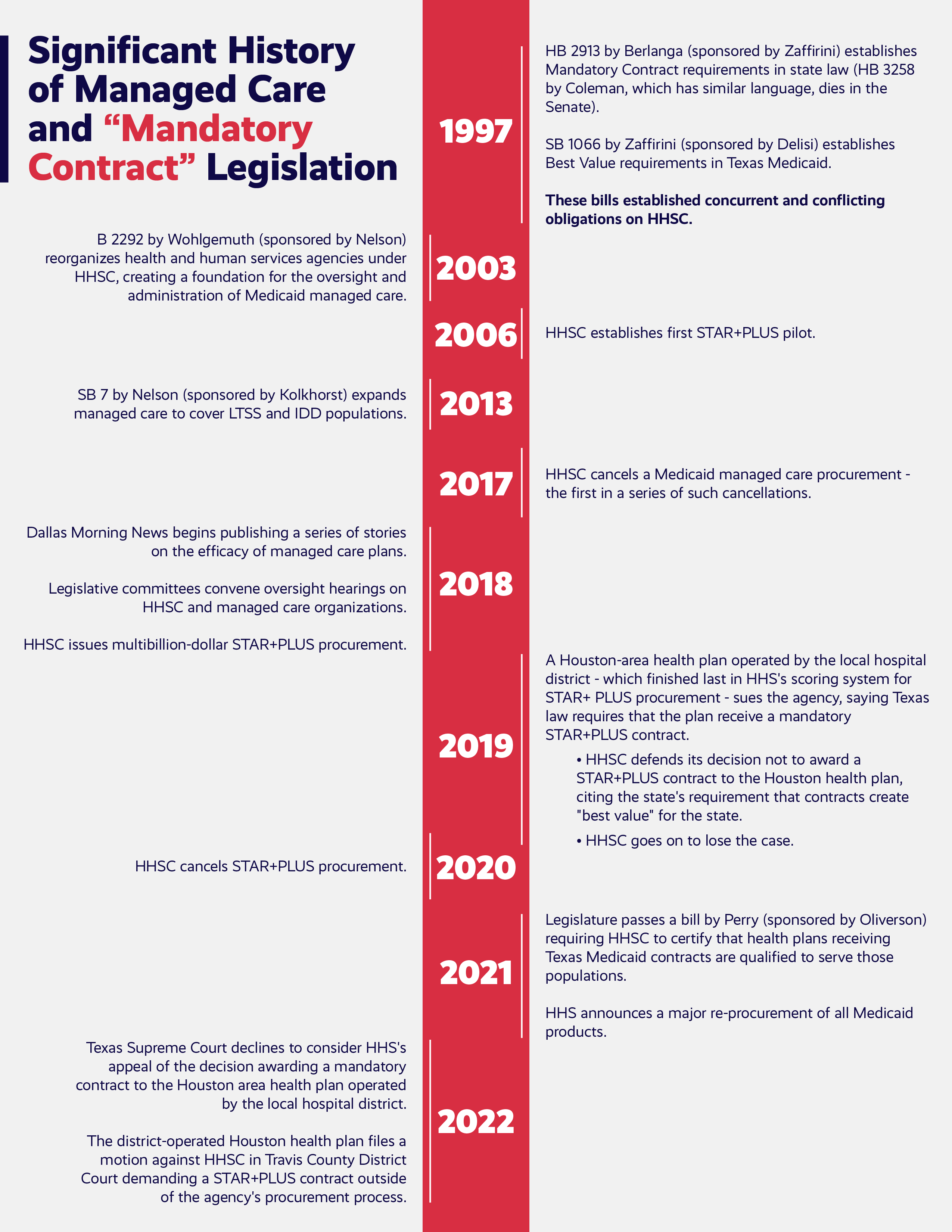
The History of Mandatory Contracts in Texas
A Texas law — passed via undebated floor amendment nearly a quarter-century ago — requires the Texas Health & Human Services Commission (HHSC) to award Medicaid managed care contracts to health plans that are controlled by local officials in big Texas counties through special districts empowered to tax constituents to fund public hospitals.
- Texas courts have ruled that only the legislature can change this law.The Legislature created Mandatory Contracts in the early years of Texas’ Medicaid managed care system to protect public hospital systems from uncertainties associated with this new managed care model.
- Those uncertainties no longer exist: HHSC spends nearly $33 billion a year on managed care.
- Public hospitals and clinics in big Texas cities receive billions more through Texas’ 1115 waiver specifically to provide care to indigent (uninsured) patients.
What Has Changed
Health plans controlled by taxing hospital districts and urban counties have begun pursuing contracts to manage complex Medicaid services for the most vulnerable Texans — even though HHSC has concluded some lack the experience, expertise, and resources (or resource capacity) necessary to manage these contracts.
- Courts agree that, under this antiquated state law, county-controlled health plans do not have to meet state standards or compete through the managed care system.
County-controlled health plans defend their special status by pointing to the role of county-wide taxing districts in providing indigent care and intergovernmental transfer money for federal Medicaid funding.
Yet hundreds of public hospital districts help the state draw down Medicaid funds; only five currently have health plans with the special privilege of guaranteed Medicaid contracts.
- Indigent care obligations relate only to districts’ ability to collect property taxes — they have nothing to do with protections for health plans controlled by officials in Texas’ biggest counties.
The counties’ own arguments show these health plans exist primarily to create more revenue for county governments and hospital districts, not provide the best care or meet HHSC goals.
The Future
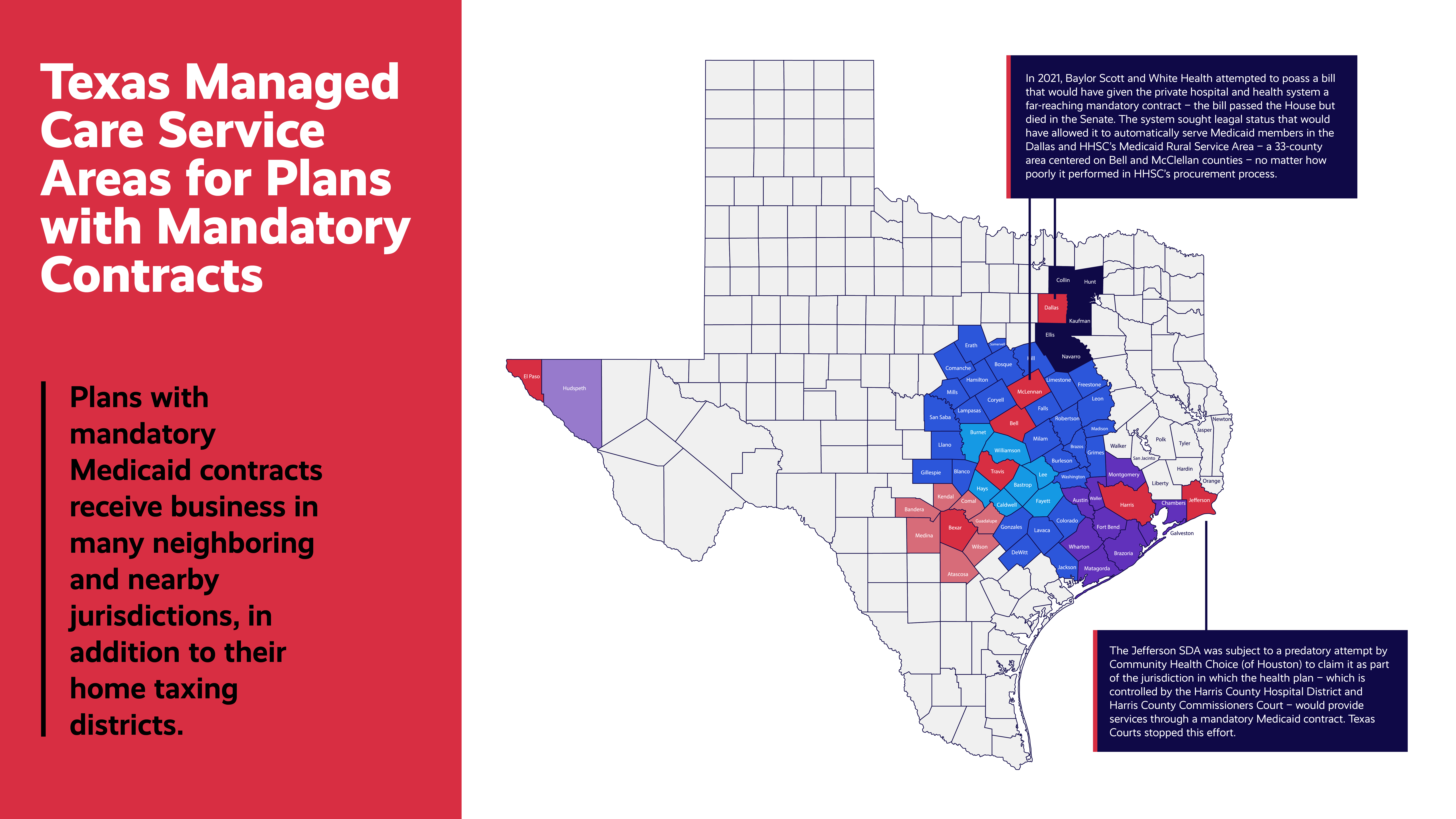
If allowed to stand, urban county governments and taxing hospital districts will seize more and more Medicaid responsibilities away from HHSC.
- The state will lose the ability to operate the state’s managed care system in a way that protects Medicaid members and Texas taxpayers.
This will likely trigger higher local property taxes and state Medicaid costs.
- It also will create a patchwork of single payer-style Medicaid systems — not the competitive, market-driven model that Texas pioneered.
